What is diabetes?
Diabetes mellitus (DM) is a group of metabolic disorders characterised by elevated glucose levels in the blood (hyperglycemia), which result from defects in insulin secretion, action, or both.
The food that we eat is broken down and converted to glucose. Glucose is necessary for our body’s cells to function properly. Insulin is a hormone secreted by the pancreas, and it regulates the metabolism of glucose in the body. Insulin promotes the uptake of glucose by different cells and its storage in the liver. If the uptake and utilisation by cells are hampered, then the glucose levels in the blood increase, resulting in hyperglycemia.
Prolonged hyperglycemia damages the blood vessels, resulting in complications such as heart disease, kidney disease, and blindness
What are the types of diabetes mellitus?
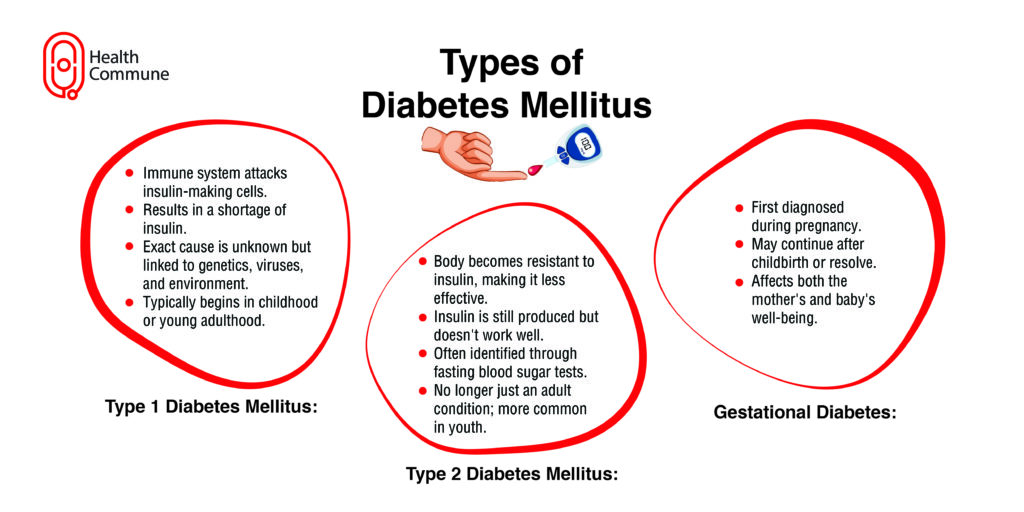
Diabetes can be further divided into:
- Type I diabetes mellitus: The exact cause of type I DM is unknown. Usually, the cells of the pancreas that produce insulin (β cells of pancreatic islets) are destroyed by the body’s immune system, resulting in a lack of insulin. Other possible causes include genetics, viral infections, and exposure to certain environmental factors
- Type II diabetes mellitus: Characterised by a relative insulin deficiency and resistance of cells to insulin. A Blood test reveals fasting hyperglycemia regardless of the availability of insulin
- Gestational diabetes: Diabetes is diagnosed for the first time during pregnancy. It may or may not go away after childbirth. Gestational diabetes can impact both the mother’s and the baby’s health
What is pre-diabetes?
What causes type II diabetes?
The hyperglycemia in type II diabetes mellitus may be due to:
- Impaired insulin secretion: β cells of pancreatic islets are exhausted due to overuse, resulting in too little secretion
- Peripheral insulin resistance: Increased visceral fat (fat stored within our body that surrounds and protects our internal organs) prevents the uptake of insulin by cells
- Increased production of glucose by the liver due to impaired suppression
What risk factors contribute to type II diabetes mellitus?
- Age : older than 45 years
- Having a body mass index ≥ 25
- High blood pressure (blood pressure ≥ 140/90 mm of Hg)
- High cholesterol levels in the blood
- Gestational diabetes mellitus
- Family history of diabetes
- Previous history of a heart attack or stroke
- Asian race
- Inactive lifestyle
- Pre-diabetes
What are the symptoms and warning signs of type II diabetes mellitus?
- Increased hunger
- Increased thirst
- Frequent urination
- Fatigue and tiredness
- Numbness and tingling sensation of the feet
- Unexplained weight loss
- Wounds that take a very long time to heal
- Blurred vision
- Vaginal infections in women
- Sexual dysfunction
- Gum infections
How is type II diabetes mellitus diagnosed?
- Blood tests:
- Fasting blood sugar level (after overnight fasting of at least 8 hours),
- post-prandial blood sugar (2 hours after eating)
- HbA1C (Glycosylated haemoglobin level which reveals your average blood glucose levels over the past 3 months)
- Oral glucose tolerance test (OGTT) You’ll be asked to fast overnight (10 to 12 hours) and have an unrestricted diet (more than 150 g of carbohydrate daily) for at least 3 days before this. You’ll be given a solution containing 75 g of glucose in 150 – 300 mL of water and your blood samples are drawn periodically to see your response to glucose (once during the fasting period and then 2 hours after the test load).
| Fasting blood sugar (mg/dL) | Post-prandial blood sugar (mg/dL) (after 2 hours) | HbA1C | Oral Glucose Tolerance Test (mg/dL) | |
|---|---|---|---|---|
| Normal | 70-100 | 70-140 | <5.7% | 70-100 |
| Prediabetes | Between 100 and 126 | Between 140 and 200 | 5.7% to 6.4% | Between 140 and 200 |
| Diabetes | ≥126 | ≥200 | ≥6.5% | ≥200 |
- Urine test : For glucose, proteins, ketone bodies, and signs of infection in urine
How is type II diabetes mellitus treated?
Diabetes, in many cases, is a lifestyle disease, and hence its management is not just limited to medicines but an overall change in lifestyle. This includes:
- Dietary modifications
- Eat 5–6 small meals at regular times every day
- Do not skip meals as this may result in overeating at your next meal
- To lose weight, cut down the portion size
- Eat a wide variety of foods every day
- Eat high-fibre foods: fruits, vegetables, grains, and beans
- Use less added fat, sugar, and salt
- Avoid potatoes, sweets, and fried food
- Exercise
- Make regular exercise a part of your routine
- Exercise could be in the form of being extra active every day, taking the stairs, walking while talking on the phone, etc.
- Doing aerobic exercise such as more than 30 minutes/day of swimming, cycling, brisk walking, etc.
- Doing strength training: Building muscle helps because muscle burns more calories than fat
- The Indian Council of Medical Research (ICMR) recommends yoga for diabetes management as well
- Medicines
Insulin: Insulin therapy is essential for replenishing the insulin your body is unable to make if you have type 1 diabetes. When alternative therapies fail to keep blood glucose levels within the recommended range, persons with type 2 diabetes or gestational diabetes may occasionally need insulin therapy. By maintaining your blood sugar levels within your goal range, insulin therapy helps prevent diabetic complications. The types include long, ultralong, or intermediate-acting insulin and short or rapid-acting insulin.
Oral anti-diabetic medicines: These drugs lower blood sugar in a variety of ways, including by stimulating the pancreas to generate more insulin. The category of drugs includes:
Alpha-glucosidase inhibitors: These work to lower blood sugar levels by preventing the breakdown of starches and some forms of sugar in your intestines. E.g., acarbose and miglitol
Biguanides
They reduce blood sugar levels by limiting the quantity of glucose your liver generates and releases into your bloodstream.
E.g., metformin
Bile acid sequestrants (BASs)
Low-density lipoproteins, also known as LDL cholesterol or “bad” cholesterol, are removed by Bile Acid Sequestrants. The medication stops your stomach’s bile acid from entering your bloodstream. E.g., colesevelam
DPP-4 inhibitors (gliptins)
Gliptins, or DPP-4 inhibitors, work to lower blood sugar levels by stopping the body from breaking down a substance called GLP-1 or glucagon-like peptide (amino acid long peptide hormone).
E.g., sitagliptin and saxagliptin
Meglitinides (glinides)
Meglitinides are drugs that encourage the secretion of insulin from your pancreas.
Eg: Nateglinide and Repaglinide E.g., nateglinide and repaglinide
SGLT2 inhibitors
By facilitating the removal of excess glucose from your body through urination, these drugs lower blood glucose levels (urine).
Eg:Canagliflozin and dapagliflozin E.g., canagliflozin and dapagliflozin
Sulfonylureas
Your pancreas releases more insulin when you take sulfonylureas. You’re more likely to experience low blood sugar as a result of their increased insulin production (hypoglycemia). E.g., glimipiride, glipizide
Thiazolidinediones (TZDs)
Your muscle and fat tissues are made more sensitive to insulin by these categories of drugs. They also reduce the liver’s ability to produce glucose.
E.g., rosiglitazone
Injection medicines that are not insulin: It keeps food in the stomach longer, increases insulin when you eat and also reduces the amount of glucose released by the liver
examples include Exenatide, Liraglutide
What are the complications of type II diabetes mellitus?
Acute complications (rapid-onset complications)
1.Hypoglycemia
2.Blood sugar level falls below 70mg/dL
3.Occurs in those taking tablets or insulin injections for the treatment of diabetes
Causes of hypoglycemia could be due to:
1. Exercising more than usual
2. Delaying or omitting a snack or a main meal
3. Administration of too much insulin
4. Taking an incorrect dose of your medicine
5. Overindulging in alcohol
Symptoms include sweating, rapid heartbeat, trembling, nervousness, irritability, hunger, headache, confusion, blurring of vision, loss of memory, seizure, loss of consciousness and even coma in severe cases
Treatment : In mild cases, consuming 15 – 20 g of glucose, candy, sugar, or fruit juice will resolve the symptoms; however, severe hypoglycemia might require hospitalisation and intravenous (IV), intramuscular (IM), or subcutaneous delivery of glucose
- Diabetic ketoacidosis
1.This condition occurs more frequently in people with type I diabetes and rarely in type II DM
2. The absence of insulin leads to increased breakdown of proteins and fats making the blood acidic
3. The excess glucose in the blood is eliminated through the kidneys which results in frequent urination, loss of minerals, and salts in urine and dehydration
4. A person with diabetic ketoacidosis typically has a fruity breath, confusion, and sometimes loss of consciousness
5. Once identified, the person has to be immediately admitted to the hospital for management of the condition - Hyperglycemic hyperosmolar nonketotic syndrome
1. This occurs due to a relative insulin deficiency and presents as dehydration that can progress to coma if not treated
2. The person should be immediately admitted to the hospital for management - Chronic complications (these occur gradually over the years)
1. Cerebrovascular disease
2. Heart disease
3. Peripheral artery disease
4. Ulcers which don’t heal
5. Kidney disease (diabetic nephropathy)
6. Damage to retina (diabetic retinopathy)
7. Damage to nerves (diabetic neuropathy)
8. Diabetic foot
How can I prevent type II diabetes mellitus?
- Eat a healthy meal rich in fruits and vegetables. Minimise the intake of food substances rich in sugar and fat
- Exercise frequently
- Undergo routine screening tests to ensure that diabetes will be detected early



