Pancreatitis may strike you suddenly or develop gradually. learn to know more about its causes, risk factors, symptoms, and treatment.
What is the pancreas?
The pancreas is an organ that is located in your abdomen, behind your stomach. This organ has two functions:
- It produces and releases enzymes that help in digestion
- It produces and releases hormones that control and regulate glucose levels in the body
What is pancreatitis?
Swelling of the pancreas is called pancreatitis. If the swelling occurs suddenly and lasts for a few days, it is called acute pancreatitis. Acute pancreatitis occurs as a result of a sudden injury to the pancreas. Swelling of the pancreas that occurs over many years is called chronic pancreatitis.
What causes pancreatitis?
Causes of pancreatitis include
- Alcohol abuse
- Obstruction of the pancreatic duct due to cancer, gallstones or trauma
- Genetic conditions such as cystic fibrosis and hereditary pancreatitis
- Autoimmune conditions such as systemic lupus erythematosus (SLE) or autoimmune pancreatitis
- Injury to the pancreatic duct
- Trauma
- High blood calcium levels
- High cholesterol levels
- After certain medical procedures (endoscopic retrograde cholangiopancreatography, abdominal surgery)
- Medicines (azathioprine, 6-mercaptopurine, ACE inhibitors used for treating high blood pressure, valproic acid, didanosine, and mesalamine)
- Genetic factors
- Infections, including viral, bacterial, and parasitic infections
- Kidney diseases
- Poisoning (for example, scorpion bite, consumption of pesticides or insecticides – organophosphorus poisoning)
What are the risk factors for pancreatitis?
Risk factors include:
- Alcoholism
- Smoking
- Obesity
- Family history of gallstones or pancreatic diseases
What are the symptoms of pancreatitis?
The most common symptoms include:
- Moderate to severe, sharp pain in the upper part of the abdomen that radiates to the back
- Nausea and vomiting
- Fever
- Rapid heart rate
- Pain on touching the abdomen
How is pancreatitis diagnosed?
Your doctor will first inquire about the history of symptoms and potential causes that may have resulted in pancreatitis. As a part of the physical examination, your doctor may press your abdomen to understand the exact location of the pain. In addition, you might be asked to undergo the following tests:
- Blood tests that measure your digestive enzymes, blood sugar levels, etc.
- Stool test
- Ultrasound or CT scan
- Endoscopic ultrasound: (a thin and flexible tube with a small ultrasound probe is passed into your stomach through the throat to better visualise the pancreas, part of the liver, gallbladder, and bile duct)
What are the complications of pancreatitis?
If untreated, pancreatitis may lead to the following complications:
- Breathing problems (acute respiratory distress syndrome)
- Kidney failure
- Diabetes
- Digestive problems such as malnutrition, diarrhoea, and weight loss
- Cancer
- Pseudocyst (collection of debris and fluids in cyst-like pockets in the pancreas) Infections
How is pancreatitis treated?
The initial phase of treatment is aimed at controlling the pain and inflammation. This includes:
- In-hospital monitoring and intravenous fluids
- Pain control through medications
- Endoscopic procedures to remove gallstones or any other kind of blockage
- Surgical removal of a part or the whole part of the pancreas
- Insulin injections to control blood sugar levels
How will surgical removal of the pancreas impact my life?
You can survive without a pancreas and still be healthy. However, you may have to be on insulin therapy for the rest of your life (since insulin is produced by the pancreas, a lack of insulin would result in diabetes). Additionally, dietary modifications, including following a low-fat, low-sugar, and low-carbohydrate diet and eating multiple small meals across the day instead of two or three large meals, would be required.
What is endoscopic retrograde cholangiopancreatography (ERCP)?
Narrowing or blockage of the pancreatic duct or bile duct may be the cause of pancreatitis in some cases. ERCP is done to diagnose and treat these conditions.
In ERCP, your doctor passes a thin, flexible tube called an endoscope down your throat, through your stomach , and into the first part of your intestine called the duodenum. A small video camera fitted to the endoscope captures the images during the procedure. Once the ducts are located, a tube called a catheter is passed through the endoscope, and a dye (contrast medium) is injected into the ducts. This dye makes the ducts more visible in X-rays. After the dye is injected, X-rays are taken to determine if there is any narrowing of the ducts. Doctors can also pass tiny tools through the endoscope to remove the obstruction, break small stones, obtain a sample for cells for further tests, or even insert stents to open the narrowed ducts.
This procedure usually takes up to 1-2 hours and is performed under anaesthesia.
Is pancreatitis curable?
Acute pancreatitis usually resolves with treatment.
In long-standing chronic pancreatitis, the inflammation may damage the pancreas permanently. This means you may have to rely on insulin injections to control your sugar levels. You may need to take pancreatic supplements to support digestion as well.
How can I prevent pancreatitis?
You can prevent pancreatitis by:
- Eating a healthy diet
- Maintaining a healthy weight
- Avoiding heavy alcohol consumption
- Avoiding smoking
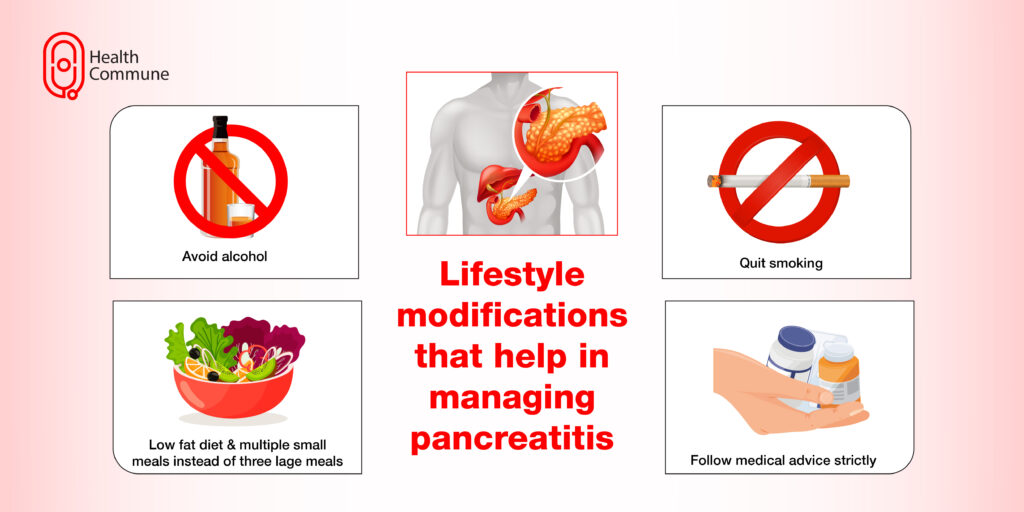
What lifestyle modifications can help in treating pancreatitis?
Some measures include:
- Dietary modifications (low-fat diet, six to eight small meals instead of three large meals)
- Avoiding alcohol
- Abstaining from smoking
- Adhering to the treatment and regularly following up with your doctor


