What is a Left Ventricular Assist Device?
A Left Ventricular Assist Device (LVAD), also called a ventricular assist system, is a mechanical device that is surgically implanted inside the chest of patients with end-stage heart failure.
The human heart has four chambers. The upper chambers are called the atria and the two remaining lower chambers are called the ventricles. The atria and the ventricles are further divided into right and left chambers.
LVAD does not replace the heart but helps the heart’s weakened left ventricle, which is the major pumping chamber of the heart, to receive and supply blood.
LVADs are usually recommended for patients who have end-stage heart failure and do not respond to medicines and for those waiting for a heart transplant.
What are the types of ventricular assist devices?
- Left Ventricular Assist Device: this helps the left ventricle pump blood to the aorta, the major blood vessel that carries blood to the whole body. This is the most commonly used type of ventricular assist device
- Right Ventricular Assist Device (RVAD): this helps the right ventricle pump blood to the pulmonary artery, the main blood vessel that carries blood to the lungs. RVAD is usually used for a short time after LVAD surgery or other heart surgery to support the right ventricle
What are the indications of LVAD?
- Bridge-to-Transplantation: Provides support for patients who are eligible for heart transplantation until a suitable donor is available
- Destination therapy: Improves the quality of life and survival rate of patients with heart failure who are not eligible for a heart transplant
- Bridge-to-Decision: Useful as a temporary support measure for patients who have some relative contraindication for a heart transplant (poor kidney function or nutritional status etc.), until they become fully eligible for receiving a transplant
- Bridge-to-Recovery: Offers temporary support to heart ventricles while weakened heart muscles recover
How does an LVAD work?
LVAD does not replace a heart, it assists the patient’s own heart by reducing the load on the left ventricle. It helps pump blood from the left ventricle to the aorta, which then supplies blood to different parts of the body.
The LVAD device has an implanted pump unit, a controller, and an energy or power supply. One end of the LVAD is attached to the left ventricle and the other to the aorta. Blood flows from the ventricles into the pump. When sensors indicate that LVAD is full, the blood is ejected out of the device into the aorta.
The controller and power supply are outside the body, and they are connected to the main pump via a cord that passes through the skin on your abdomen. The power supply consists of two batteries. If you remove both batteries simultaneously, the device will stop functioning. Hence, you have to remove them one by one.
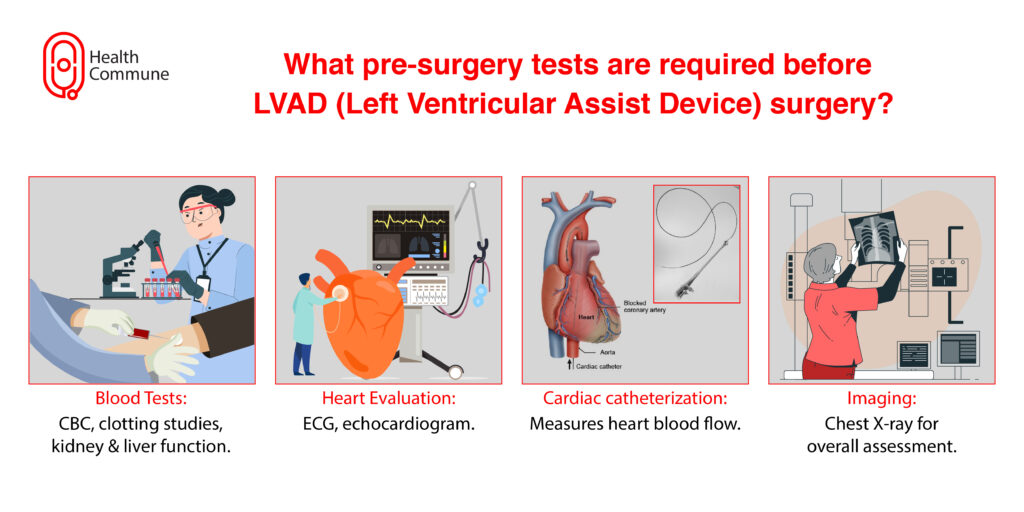
What tests would I be required to undergo before LVAD surgery?
If you are found to be eligible for an LVAD, before the surgery you will be asked to undertake the following tests:
- Blood tests: A complete blood count, bleeding and clotting studies, kidney and liver function tests
- Heart evaluation studies
- electrocardiogram (ECG)
- echocardiogram
- cardiac catheterisation: Your doctor will insert a thin, flexible tube called a catheter into your blood vessels and guide it to your heart under the guidance of X-rays. This is to measure the blood flow and pressure in your heart
- Chest X-ray
What are the preparations before LVAD surgery?
A multidisciplinary team of professionals consisting of heart surgeons, anaesthesiologists, and surgical nurses will guide you through the process.
LVAD is an open-heart surgical procedure. You will be asked to refrain from eating and drinking for at least 8 hours before the procedure.
You will be asked to sign a consent form that explains the procedure, its risks, and complications.
You will have to remove your clothing, jewellery, and other objects that may interfere with the procedure, and change into a hospital gown. Additionally, you may also be required to remove any spectacles, contact lenses, dentures, and nail polish before your procedure.
What happens during LVAD surgery?
The entire surgery happens under general anaesthesia, which means that you will sleep through the procedure.
Your heart will be stopped using medicines, and you will be connected to a heart-lung bypass machine, which ensures a continuous supply of oxygen-rich blood to all organs. You will be connected to a ventilator that will help you breathe as well.
The surgeon will cut (incision) into your chest and separate your chest bone and rib cage to access your heart.
There are various components to an LVAD. The main pump is implanted into the heart’s tip. A flexible plastic tube pumps blood to the body’s major artery (aorta). Blood is delivered to the rest of the body through the aorta. The mechanical pump is connected to a control unit and battery pack outside of your body by a cord that is inserted through your skin.
Once the main pump is implanted and found to be functioning properly, the heart-lung bypass machine will be taken off, allowing the device to pump blood.
What happens after LVAD surgery?
After the surgery, you will be shifted to the ICU for further monitoring. Medicines and fluids will be given through drips (intravenous administration). You will be connected to a ventilator to help you breathe. Tubes that drain fluid from the heart and lungs will be attached to the chest. You will also be attached to tubes to drain urine from the bladder.
You will be shifted to a normal room and eventually discharged after you regain your strength and recover.
You will have weekly check-ups in the initial period after LVAD surgery for almost a month. You will require fewer follow-up visits as you recover.
If you are waiting for a donor for a transplant, you will be in constant contact with your hospital during this period.
What will my life be like after LVAD surgery?
With LVAD, you will be able to go back to your normal life gradually with certain restrictions.
You will be on blood thinner medicines while you are on LVAD.
The external unit of the LVAD device is not waterproof. Hence, you will not be able to swim; you will have to use a special shower kit to protect the device while you shower. You will be allowed to shower only after the wound from the surgery heals completely.
You will be advised to start light exercises and strength training.
What is the life expectancy of a patient with LVAD?
What are the complications of implanting and using LVAD?
- Bleeding during or after the surgery
- Blood clots
- Destruction of blood cells (haemolysis) due to technical problems in the device
- Right heart failure
- Infections
- Stroke
- Ventricular arrhythmia (abnormal or irregular heartbeats originating at the ventricles)
- Device failure and malfunction
What are the benefits of an LVAD?
Lesser symptoms of heart failure: LVAD supports the blood flow in a person whose heart is weakened by heart disease, thus reducing symptoms, such as fatigue and shortness of breath.
Improved quality of life: It enhances the efficiency of other organ functions and improves exercise performance. Patients can take part in activities that were previously restricted due to heart failure.
Greater life expectancy: Patients who were unresponsive to medicines tend to have a longer life expectancy with LVAD.


