Do you think you might have a peptic ulcer? We’ve got everything you need to know what it is, it’s caused, the symptoms, diagnosis, treatment, and prevention.
What is a peptic ulcer?
A peptic ulcer is a sore that develops when there is a break in the inner lining of your stomach or the first part of your small intestine (duodenum).
How does it develop?
Normally, there are two types of opposing forces in your stomach:
- Damaging forces such as your stomach acid or the enzymes that help break down food
- Protective forces that include your stomach’s rich blood network as well as substances like mucus and bicarbonates, which neutralises and protect from the damage caused by stomach acid
What are the causes of peptic ulcers?
These are majorly caused by H. pylori and Non-steroidal anti-inflammatory drugs (NSAIDs).
- H. pylori is a spiral-shaped bacteria that can infect your stomach and small intestine
- Regular use of NSAIDs, a group of painkillers that include high-dose aspirin, and ibuprofen
- Smoking
- Alcohol
- Excessive acidity (in conditions such as Zollinger-Ellison syndrome, and parietal cell hyperplasia)
What’s the difference between gastritis and peptic ulcer disease?
Gastritis involves inflammation, redness, and irritation in your stomach’s inner lining. When this inflammation happens for a long period, it eventually causes the lining to get damaged and break down, leading to the formation of a peptic ulcer.
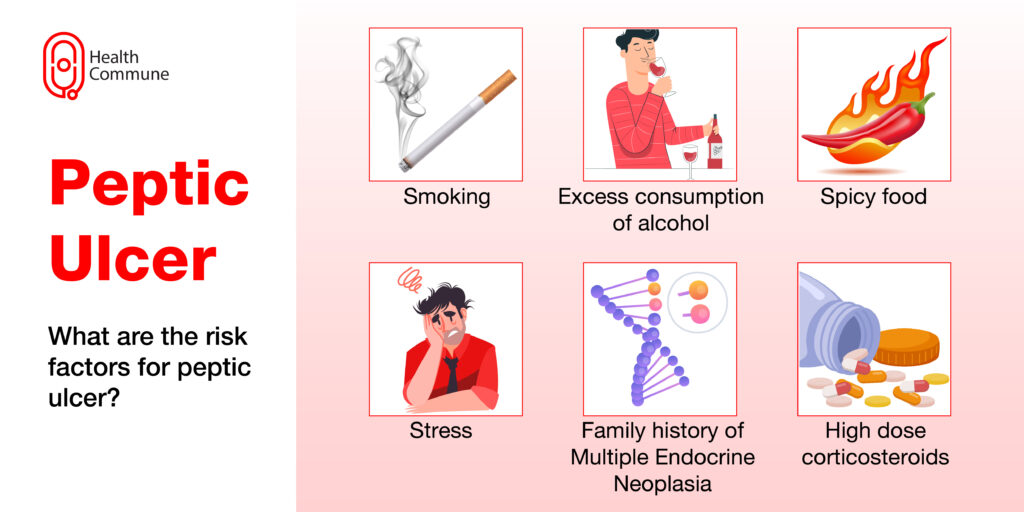
Am I at risk of getting a peptic ulcer?
You’re at a greater risk if:
- You regularly smoke
- You regularly consume alcohol
- You eat a lot of spicy food
- You’re stressed out a lot
- You regularly take high-dose corticosteroids
- You have a family history of conditions such as multiple endocrine neoplasia 1 (MEN 1)
What are the symptoms of peptic ulcers?
You may experience:
- Burning or gnawing type of stomach pain, which can radiate to other parts of the abdomen or your back
- If the sore is in stomach (gastric ulcer), you may notice that pain gets worse after eating and you might develop an aversion to eating
- If the sore is in small intestine (duodenal ulcer), eating might seem to relieve pain, and as a result, may be eating more
- Heartburn
- Nausea
- Excessive saliva in your mouth
- Loss of appetite
- A feeling of fullness, or bloating sensation
When do I need to see a doctor?
Visit your doctor immediately in case you notice signs of bleeding, such as:
- Blood in your vomit
- Blood in your stools, or dark-coloured stools
How is a peptic ulcer diagnosed?
Your doctor will ask you for a thorough history of your symptoms. To confirm the diagnosis, they will recommend:
- Tests for H. pylori: To detect the presence of H. pylori in your stomach, your doctor will recommend a blood, stool, or urease breath test
- Endoscopy: A thin, long tube with an attached camera is inserted through your mouth to confirm its presence and location
- Barium swallow: In this, you’ll be asked to swallow a radioactive liquid, and a series of x-rays will then be taken to visualise your gastrointestinal tract
- Biopsy: Your doctor can take a small piece of tissue from the affected site in case they suspect cancer
How is peptic ulcer treated?
Based on the underlying cause, you will be prescribed:
Medicines: such as:
- Antacids, to neutralise stomach acid. These are rarely used now
- H2 receptor blockers, to inhibit the secretion of stomach acids and enzymes
- Proton pump inhibitors, or PPIs, which prevent stomach acid production. These are more popularly used nowadays
- Protective barriers, which prevent the action of stomach acid on your stomach lining and promote healing
- Antibiotics
Why are antibiotics used in peptic ulcers?
Your doctor can prescribe antibiotics in cases of H. pylori infections. This treatment usually lasts for 2 weeks and includes a combination of 3-4 medicines that include two antibiotics, one proton pump inhibitor (PPI), and occasionally a protective barrier.
Is surgery ever done for peptic ulcers?
In cases of a chronic, non-healing sore that is not responding to antibiotics or acid-suppressing drugs, or in cases of complications, surgery can be done. These include:
- Partial gastrectomy, where the part of the stomach containing the ulcer is surgically removed
- Vagotomy, where the vagus nerve (the nerve responsible for signalling to the stomach to produce acid) or its branches are cut to reduce the production of stomach acid
What are the complications of peptic ulcer?
Complications include:
- Internal bleeding from your gut
- Anaemia, in the case of chronic blood loss
- Perforation, or the formation of a hole in your gut wall, can lead to serious infections
- Obstruction in your gastrointestinal tract, not allowing food to pass through and causing electrolyte imbalances
- Pancreatitis
- Gastric cancer
Can a peptic ulcer lead to cancer?
Rarely, chronic and untreated peptic ulcers in the stomach may lead to gastric cancer. Sores in the duodenum are not associated with an increased risk of cancer.
How can I prevent peptic ulcers?
You can reduce your chances of suffering from this condition by:
- Not taking painkillers unless needed or prescribed by your doctor
- Quitting smoking and drinking
- Reducing your stress levels
- Taking general precautions to decrease H. pylori infections, such as frequent hand washing, drinking only boiled or purified water, and eating well-cooked food from hygienic places
What’s the difference between acid reflux and a peptic ulcer?
Acid reflux (medically called GERD or gastrointestinal reflux disease) is a condition where stomach acid flows backward into your oesophagus, leading to heartburn, difficulty swallowing, and coughing. Although it shares some similarities with the latter, it’s essential to differentiate between the two conditions since they have different treatments and complications.


